Study Indicates Artificial Intelligence Could Help Stem Tide of School Violence
Study Indicates Artificial Intelligence Could Help Stem Tide of School Violence
Natural Language Processing Already Used to Predict Mental Health Risks
Tuesday, April 28, 2020
By leveraging the basics of artificial intelligence (AI) technology now used to predict risk for suicide or other mental health issues, researchers developed an AI system that analyzes linguistic patterns to predict a youth’s risk for committing acts of school violence.
Study data published in the International Journal of Medical Informatics by physicians and clinical informaticians at Cincinnati Children’s show the system can detect the risk of aggression for individual subjects.
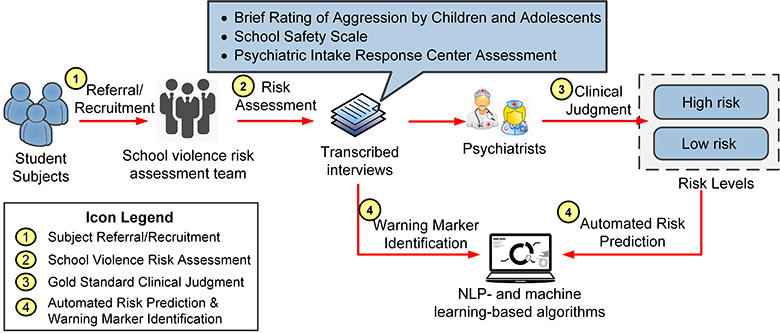
The AI system uses pattern-recognizing machine learning and natural language processing (NLP) technologies. It combines the analytical scope and speed of information technology with clinical risk-assessment data and practitioner expertise, thereby automating a complex and time-consuming process, according to Yizhao Ni, PhD, co-principal investigator and a clinical informatician in the Division of Biomedical Informatics.
The technology uncovered multiple warning signs that could deliver useful clinical insights to assist personalized interventions, Ni explained. When fully developed, the system’s built-in risk assessment scales and automated risk prediction algorithms should produce an accurate and scalable computerized screening service to prevent school violence.
“Students are physically or verbally bullied on school property, electronically through texting or social media, and youth violence costs society billions of dollars in healthcare expenses or lost productivity,” Ni said, citing data from the U.S. Centers for Disease Control and Prevention.
“Our study demonstrates that overall, our AI system matches the clinical judgements and accuracy of psychiatrists 94 percent of the time. It has tremendous potential to help address youth violence at school and eventually other mental health conditions.”
Empowering a Solution
Earlier research shows that using NLP and machine learning technologies pioneered at Cincinnati Children’s and elsewhere improve risk prediction for mental health problems like suicide. Current study authors note that so far there are no automated solutions developed to predict the risk for violent behaviors at school.
Recent advancements in school-based crime prevention programs demonstrate the best results occur when at-risk youth receive timely and individualized intervention, according to Drew Barzman, MD, co-principal investigator and director of the Child and Adolescent Forensic Psychiatry Service at Cincinnati Children’s.
But high patient need and busy clinical schedules can constrain the ability to complete the complex, labor intensive tasks needed for timely clinical evaluation of mental health patients. An effective automated system could help overcome this challenge and help mental health caregivers deliver timely interventions based on a youth’s individual needs, he said.
Contact Information
Study Design
The study was tested by embedding it as a clinical service in the Division of Child and Adolescent Psychiatry at Cincinnati Children’s. The division’s inpatient units receive about 30,000 psychiatric admissions annually. Its outpatient clinic has over 52,000 patient visits every year.
Conducted between May 2015 and April 2018, the study prospectively recruited 131 students between ages 10 and 18 years from middle and high schools in Ohio, Kentucky, Indiana, and Tennessee.
Clinical assessments by psychiatrists indicated that 68 students (52 percent) were considered high risk toward others. For analysis with the AI assessment tool, the patients were segmented into smaller groups to compare the system’s predictive reliability when compared physician-generated patient clinical assessments. These comparisons yielded the AI system’s overall risk assessment match rate of 94 percent.
Future development plans for the tool include seeking research collaborations with other medical institutions and school systems to test live implementation in educational and medical settings, according to the researchers. Researchers said that based on funding capabilities, this will be the next phase of their work.
The study was supported in part by the National Institutes of Health (1R01LM012230, 1U01HG008666, UL1TR001425), the Agency for Healthcare Research and Quality (1R21HS024983) and internal funding from Cincinnati Children’s.
Contact Information
Nick Miller
513-803-6035
nicholas.miller@cchmc.org



