How Risky Is Surgery?
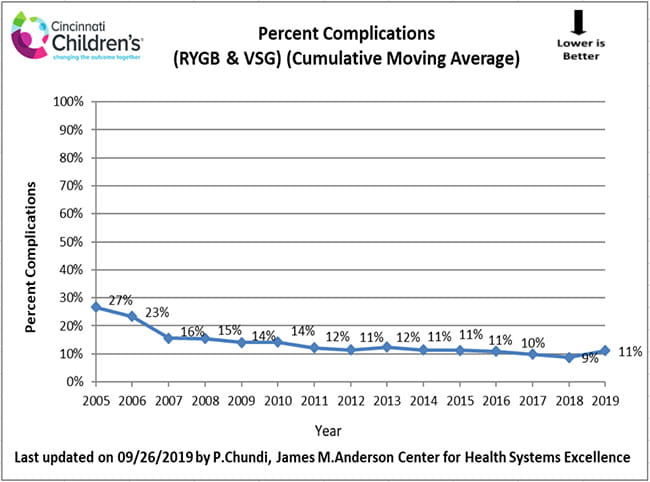
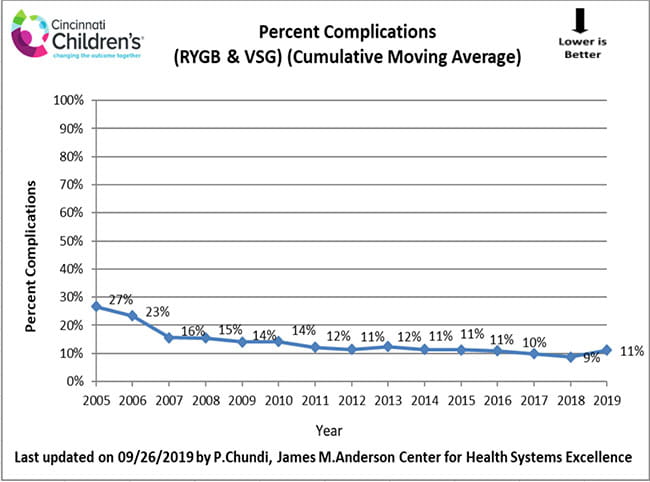
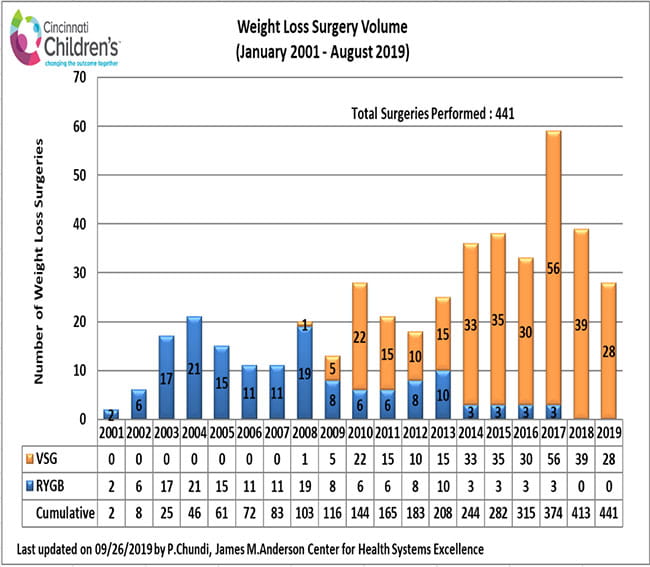
The Surgical Weight Loss Program for Teens team collects and analyzes our own results. Safety and reduction of risks associated with weight loss surgery are priorities. In the section below, we describe the complications and other adverse events or risks of treatment that can result from weight loss surgery. We monitor and analyze our complications to continually improve the care we deliver and empower families to ask questions and feel comfortable with the life-changing treatment decisions they are making.
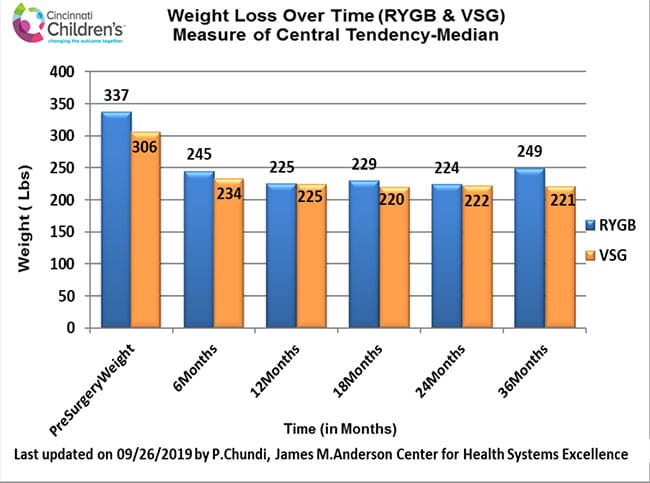
The average hospital stay for adolescents undergoing weight loss surgery is two to three days, and most patients will return to school or work within two weeks. However, as with any major surgery, both the RYGB and VSG procedures pose potential health risks in the short and long term.
Risks associated with weight loss surgery can include:
| Leak of stomach contents |
Bowel obstruction |
| Bleeding |
Gallstones |
| Infection |
Hernias |
| Adverse reactions to anesthesia |
Low blood sugar (hypoglycemia) |
| Blood clots |
Malnutrition |
|
Lung or breathing problems
|
Stomach perforation |
| Ulcer |
Ulcers |
| Dehydration |
Vomiting |
| Vitamin deficiencies |
Death (rare) |
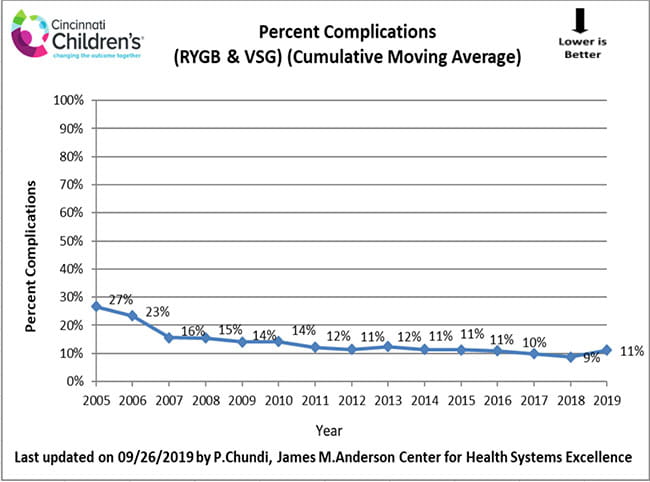
How We Measure
These data include the outcomes of patients at six weeks following weight loss surgery.
Continuous Improvement
- To decrease the amount of nausea and vomiting after sleeve gastrectomy we now apply the scopolamine patch (anti-nausea medicine) before going into the operating room.
- We worked with the hematology team to adjust the dose of Lovenox to decrease risk of bleeding while still protecting against deep vein thrombosis (blood clots).
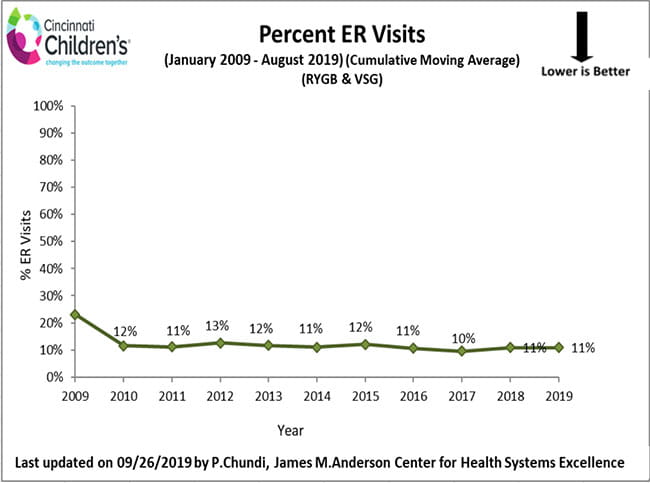
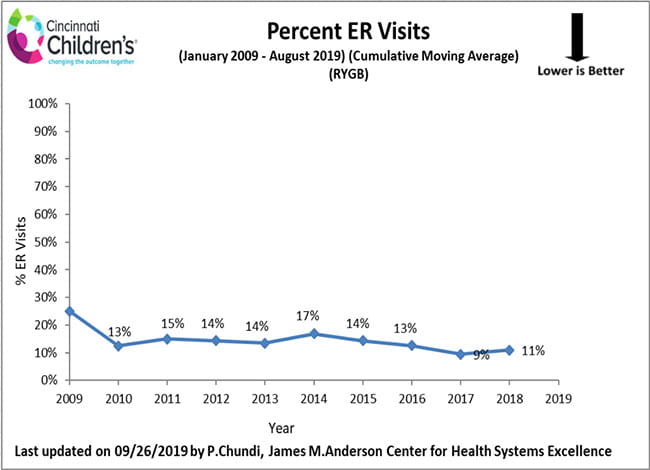
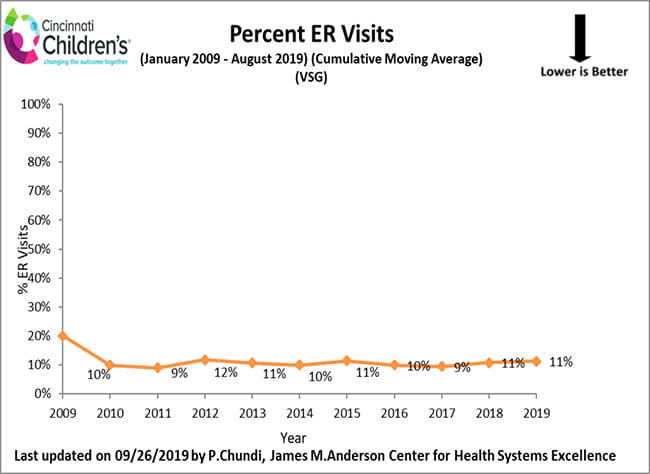
Emergency Department Visits Following Weight Loss Surgery
The charts below account for our program’s weight loss surgeries to date, and demonstrate the percentage of patients who visited the Emergency Department to address a health issue following his/her weight loss surgery. With each visit to the Emergency Department, the surgical weight loss team reviews the specifics of each patient event and develops a plan to decrease the likelihood of a reoccurrence.
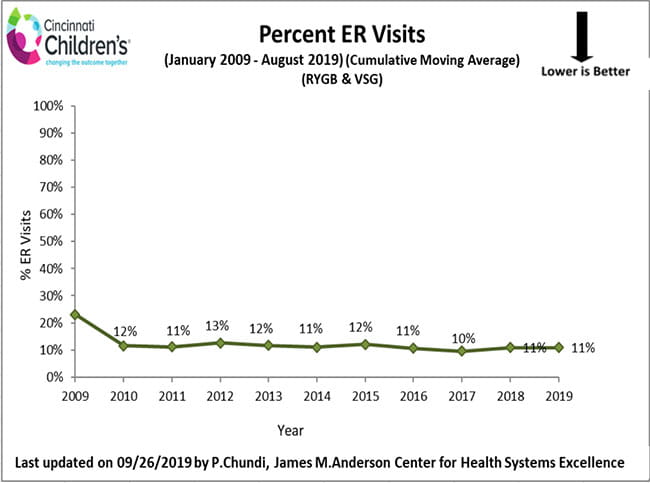
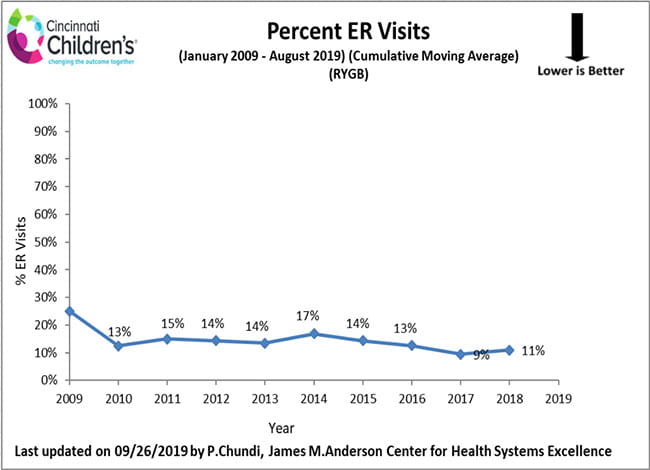
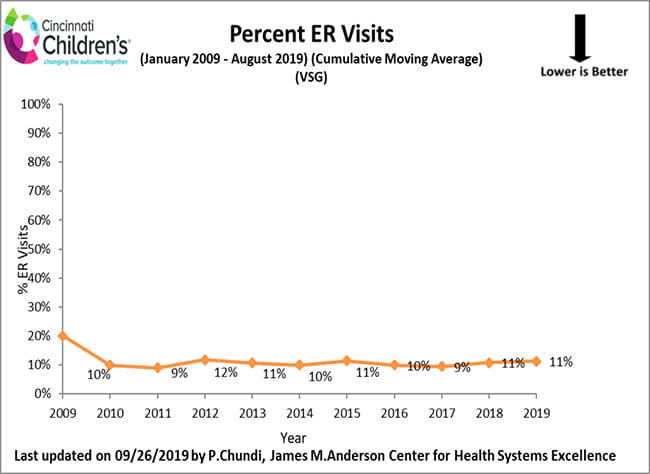
How We Measure
These data include the outcomes of patients at six weeks following weight loss surgery.
Continuous Improvement
To ensure easy access to the team for problem solving and support post-surgery, we provide all patients and families with 24-hour access to the nurse practitioner by text or phone, in addition to daily calls for the first two weeks after surgery. We have found this to be a great way to stay connected and deliver ongoing education about what to expect during this critical time. Through this process, patients are able to ask questions and discuss any concerns with the team member, which can in turn help to avoid emergency room visits.
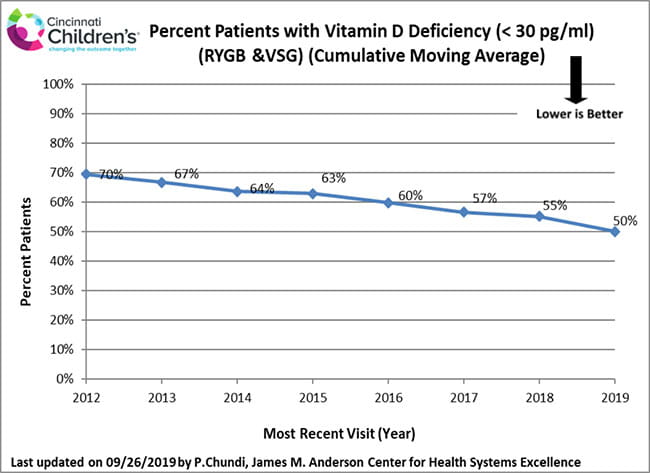
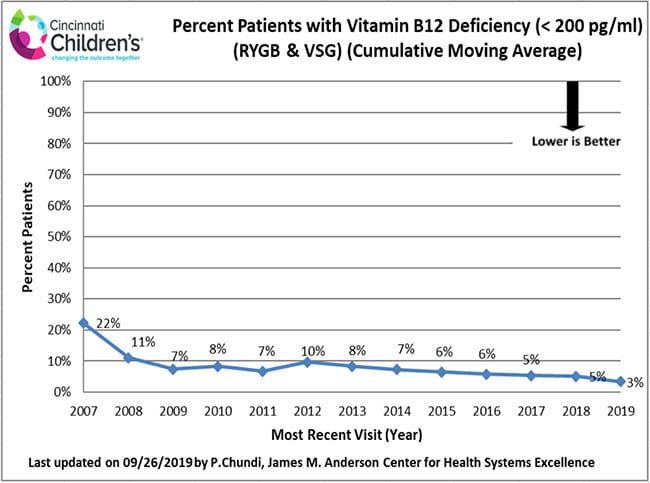
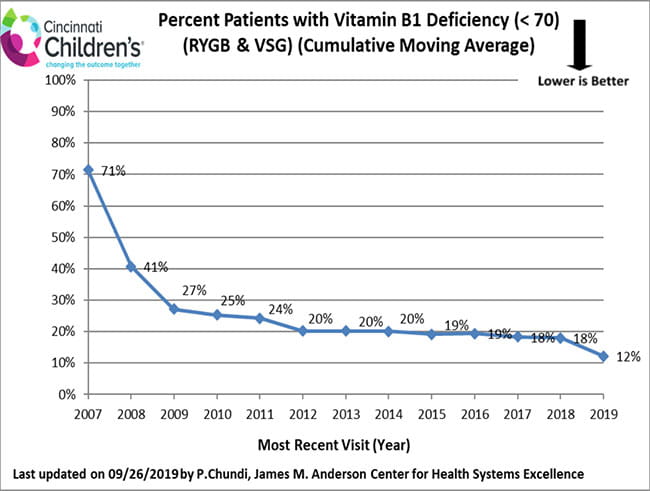
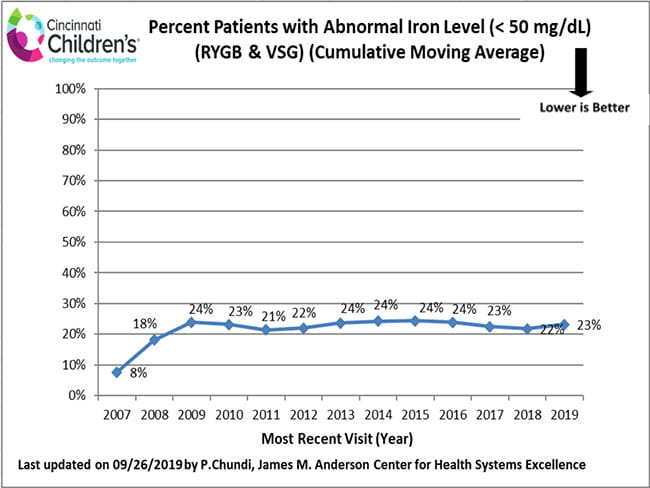
Nutritional care is an essential part of the long-term health of all weight loss surgery patients. Due to the reduction in overall food intake and absorption changes of some nutrients, vitamin deficiencies may occur in weight loss surgery patients regardless of procedure type. All SWLPT post-operative patients are carefully counseled and prescribed vitamin supplements. Laboratory testing is done at follow-up appointments to make sure vitamins are at healthy levels.
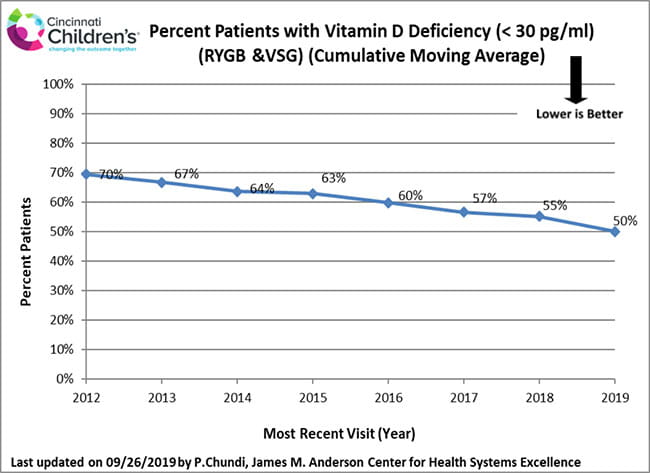
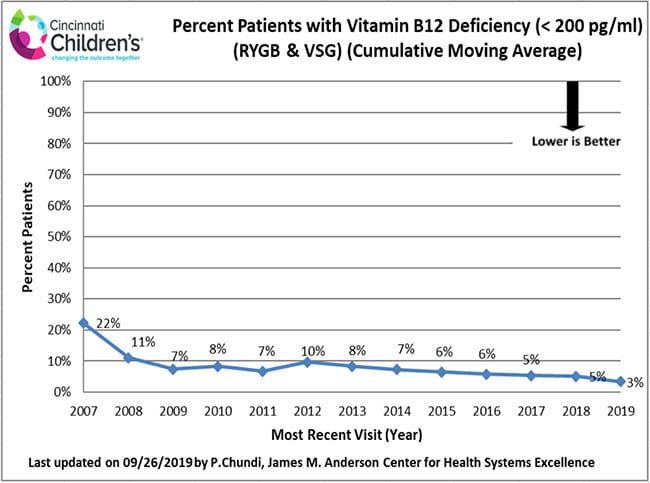
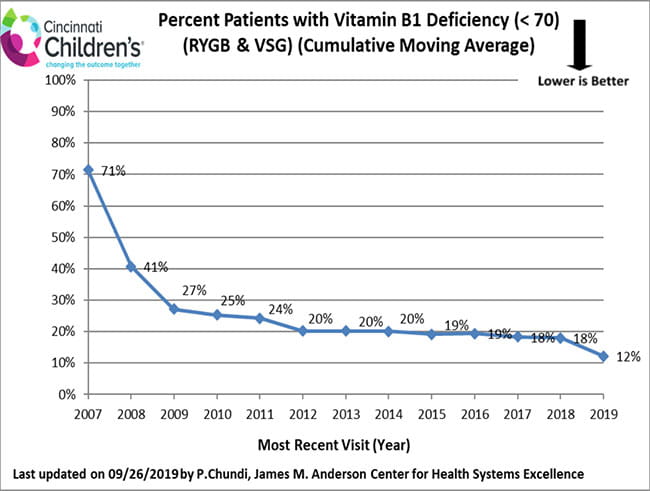
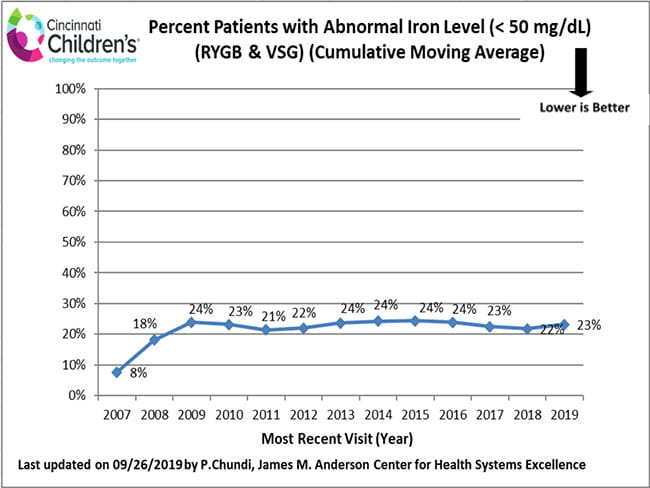
How We Measure
These data include all patients who have had a follow-up visit at least 18 months following weight loss surgery. We use this period so that enough time has passed following surgery to evaluate vitamin levels.
Continuous Improvement
- We begin supplementation with 5000 IU of vitamin D3 during the three to six months of medically supervised weight loss to treat pre-existing vitamin D deficiencies.
- We increased the dosage of vitamin D3 used to treat deficiency to 50,000 IU weekly for three months.
- We initiated an annual injection of vitamin B12 at 3000 mcg.
- All females receive consultation with gynecology before and after surgery to assist with managing heavy menstrual bleeding and prevention of iron deficiency.
- Female patients are offered the insertion of the Mirena IUD at the time of surgery.