Current Projects
As highlighted by our current projects below, our ultimate goal is to improve outcomes for people living with pulmonary disease by developing new imaging-based tools to characterize lung disease pathophysiology and to individualize clinical care.
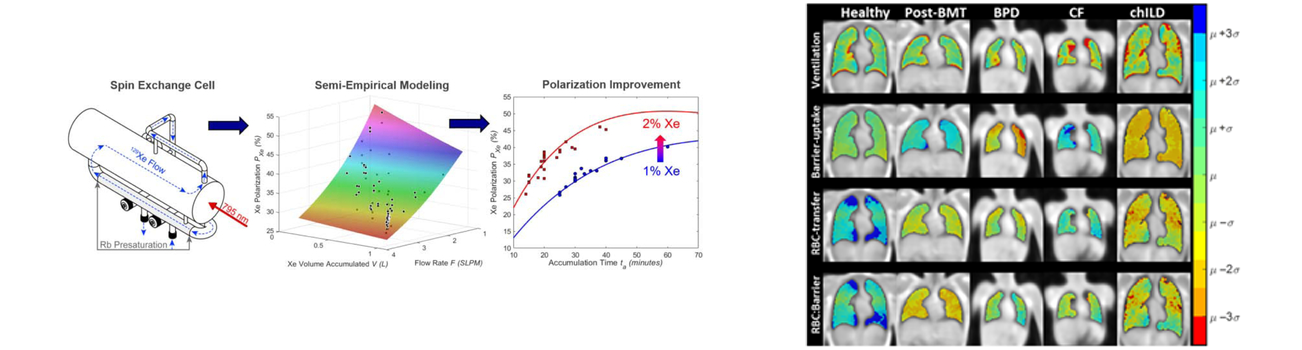
Technological and methodological developments to improve the clinical translation of Xe MRI
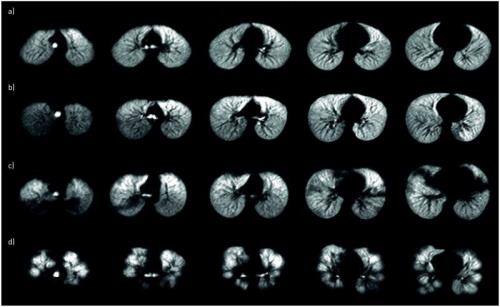
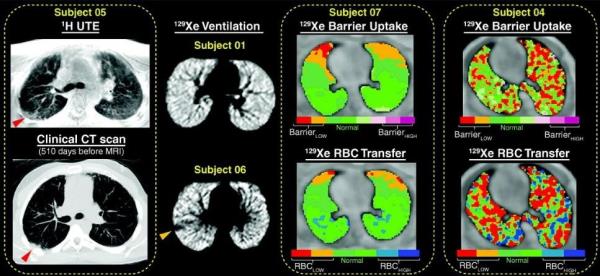
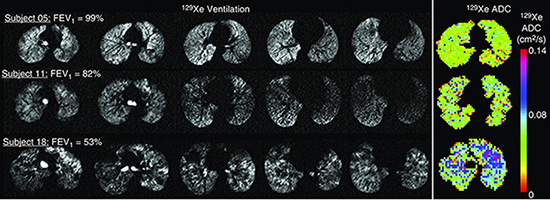
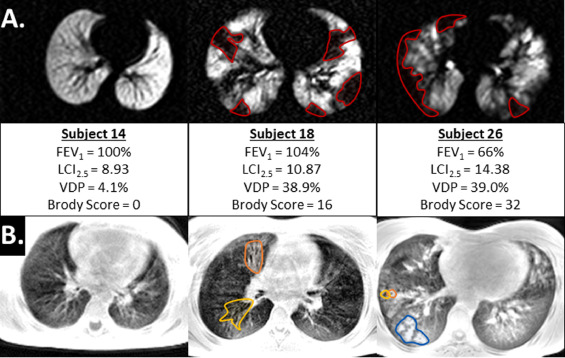
Hyperpolarized Xe gas is emerging as an inhaled contrast agent of assessing pediatric lung disease, and our group is working to improve all aspects of Xe MRI including engineering solutions for faster Xe gas production with higher MRI signal, designing MRI pulse sequences for faster acquisition with shorter breath-holds, and adapting Xe MRI techniques for younger children.
Our team was the first to demonstrate Xe MRI was safe in children and feasible even in children who are unable to perform spirometry, the clinical gold-standard test for lung disease. We recently demonstrated that Xe gas-transfer MRI, a technique that provides regional measurement of pulmonary gas exchange in adults, was feasible in pediatric populations and detected membrane-uptake and red-blood cell transfer abnormalities in children with lung disease.