
Nehal A. Parikh, DO, MS
- Attending Neonatologist, Perinatal Institute
- Professor, UC Department of Pediatrics
- nehal.parikh@cchmc.org
- Board Certified
About
Biography
I specialize in neonatology and practice evidence-based healthcare and family-centered care. More specifically, my specialties include:
- Bronchopulmonary dysplasia
- Cerebral palsy
- Cognitive impairments
- Encephalopathy of prematurity
- Neonatal hypoxic-ischemic encephalopathy
- Retinopathy of prematurity
I work with the pediatric population because of an overwhelming desire to serve vulnerable communities and because of my love for children. Due to this, pediatrics was a natural and clear choice for me. Once I learned about the great need for research into the causes and outcomes of neurodevelopmental disorders in high-risk populations, I became interested in this research area. My desire is to help these babies and their families.
While neonatology has successfully improved the survival of sick-term and preterm neonates, this medical field has made far slower progress in enhancing quality of life. This is mainly due to the high risk of perinatal/neonatal brain injury in (NICU) patients.
In my research, there are two main goals my colleagues and I are trying to accomplish. First, we are attempting to predict and diagnose neurodevelopmental conditions early in high-risk neonates. Our second goal is to foster and implement early treatment to prevent high-risk neonates from developing neurodevelopmental conditions.
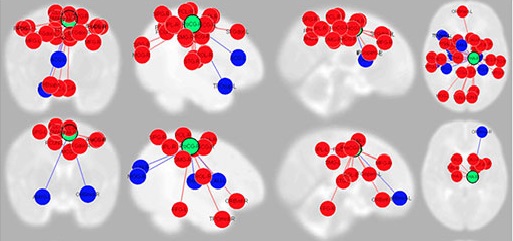
My focus as a clinician-scientist is on early diagnosis, prognosis and prevention of neurodevelopmental impairments. My colleagues and I are conducting longitudinal cohort studies of advanced magnetic resonance imaging (MRI) and neurodevelopmental results. We are looking at accelerating early detection of neurodevelopmental conditions and randomized trials of neuroprotective interventions.
In 2002, I received the Thomas Boggs Jr. Young Investigator Award during the last year of my neonatology fellowship. The Philadelphia Perinatal Society awards this honor annually to one of the top fellows from the Philadelphia neonatal-perinatal programs who has conducted the most exceptional research during their training. In 2013, I also received the Distinguished Educator Award from the neonatology fellows at Nationwide Children's Hospital, which was given to me for my commitment to teaching the fellows evidence-based medicine.
I have more than 15 years’ experience in this field and my research has received National Institutes of Health (NIH) and institutional funding since 2005. I have also used two R01 grants from the National Institutes of Health and the National Institute of Neurological Disorders and Stroke to fund the use of advanced MRI modalities, such as diffusion and functional MRI. This study explores the causes and long-term outcomes of premature infants' encephalopathy with the near-term goal of early detection of neurodevelopmental conditions.
DO: NY College of Osteopathic Medicine of NY Institute of Technology, Long Island, NY, 1996,
Residency: Pediatrics, Winthrop University Hospital of SUNY Stony Brook, Long Island, NY, 1999,
Fellowship: Neonatology, Thomas Jefferson University of Jefferson Medical College, Philadelphia, PA, 2002,
MS: Translational/Clinical Research, University of Texas Medical School at Houston, Houston, TX, 2007,
Certifications: Pediatrics, 1996; Neonatology, 2003
Interests
Evidence-based and family-centered care of very premature infants and term infants with asphyxia/neonatal encephalopathy; critically-ill newborns
Services and Specialties
Interests
Early diagnosis of perinatal brain injury/delayed brain development; early detection and prevention of neurodevelopmental disabilities
Publications
Mapping white matter microstructure at term age to motor outcomes at 2 years in very preterm infants: a multicentre cohort study. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2026.
Diffuse white matter abnormality is independently predictive of neurodevelopmental outcomes in preterm infants. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2026; 111(2):F115-F122.
MRI, General Movements, and Neurological Examination for Early Cerebral Palsy Diagnosis in Preterm Infants. Pediatrics. 2026; 157(2).
Postnatal corticosteroids and bronchopulmonary dysplasia: balancing pulmonary and neurologic effects to enable individualized decision-making. Current Opinion in Pediatrics. 2026.
Patent ductus arteriosus: emerging trial evidence firmly supports conservative management in preterm infants. Current Opinion in Pediatrics. 2026.
Postnatal dexamethasone treatment for preterm infants at high risk for bronchopulmonary dysplasia is associated with improved regional brain volumes: a prospective cohort study. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2025; 111(1):F74-F81.
Severity of punctate white matter lesions in preterm infants: antecedents and cerebral palsy prediction. Pediatric Research. 2025; 98(6):2220-2227.
Altered neurobehavioral white matter integrity in preterm children: A confounding-controlled analysis using the adolescent brain and cognitive development (ABCD) study. NeuroImage. 2025; 323:121600.
Using FRAME Documentation to Achieve RE-AIM Goals During Iterative, Stakeholder-Engaged Refinement of a Family Management Intervention for Parents of Preterm Infants. Journal of Advanced Nursing. 2025; 81(11):7690-7706.
Retinopathy of Prematurity and Risk of Structural Brain Abnormalities on Magnetic Resonance Imaging at Term Among Infants Born at Less Than or Equal to 32 Weeks of Gestation. Journal of Pediatrics. 2025; 286:114711.
From the Blog
Infection That Causes Many Preterm Births Also Linked to Developmental Disruptions
Nehal A. Parikh, DO, MS9/9/2025
Mom’s Hypertension Can Affect Preterm Infant Brain and Neurodevelopment
Nehal A. Parikh, DO, MS, Shipra Jain, MD4/30/2025
Chorioamnionitis Directly Harms the Brains of Very Preterm Infants
Nehal A. Parikh, DO, MS, Viral V. Jain, MD6/2/2022
White Matter Measure Can Predict Brain Development Risk In Preterm Infants
Nehal A. Parikh, DO, MS9/30/2020
How Novel MRI Methods Can Detect Cerebral Palsy in Extreme Preterm Infants
Nehal A. Parikh, DO, MS9/17/2019








Patient Ratings and Comments
All patient satisfaction ratings and comments are submitted by actual patients and verified by a leading independent experience management company, Qualtrics. Patient identities are withheld to ensure confidentiality and privacy. Only those providers whose satisfaction surveys are administered through Cincinnati Children’s Hospital Medical Center are displayed. Click here to learn more about our survey