What is a Brachial Plexus Injury?
A brachial plexus injury refers to an injury to the brachial plexus (BRAY-key-el PLEK-sis), a network of nerves that provides movement and feeling to the shoulder, arm and hand.
A brachial plexus injury refers to an injury to the brachial plexus (BRAY-key-el PLEK-sis), a network of nerves that provides movement and feeling to the shoulder, arm and hand.
The nerves supporting the arm exit the spinal column high in the neck; those that support the hand and fingers exit lower in the neck.
This nerve complex is composed of four cervical nerve roots (C5-C8) and the first thoracic nerve root (T1). These roots combine to form three trunks. C5-C6 form the upper trunk, C7 continues as the middle trunk and C8-T1 form the lower trunk.
Each trunk splits into a division. Half the divisions globally supply flexor muscles (that lift and bend the arm). The others supply the extensor muscles (that straighten the arm and bring it down).
A brachial plexus birth injury is thought to be caused by an injury involving the child's brachial plexus during the delivery process. This injury may result in incomplete sensory and / or motor function of the involved arm.
Per our published research, a brachial plexus injury was found to occur in 1.5 of every 1,000 live births.
Traumatic brachial plexus injuries may occur due to motor vehicle accidents, bike accidents, ATV accidents, sports, etc. Nerve injuries vary in severity from a mild stretch to the nerve root tearing away from the spinal cord.
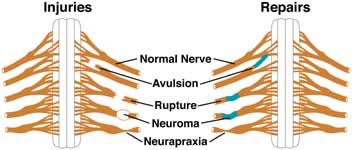
The nerve is torn away from its attachment at the spinal cord; the most severe type. An eyelid droop suggests an avulsion of the lower brachial plexus (Horner's syndrome).
The nerve is torn, but not at the spinal cord attachment.
Scar tissue has grown around the injury site, putting pressure on the injured nerve and preventing the nerve from sending signals to the muscles.
The nerve has been stretched and damaged but not torn.
The nerves of the brachial plexus originate in the neck, in the cervical spine. The nerves re-grow from the neck down the arm. This healing will occur at a rate of 1 mm per day or 1 inch per month.
A mixed or incomplete recovery may occur if the nerves do not fully reattach at their original motor and sensory targets.
Full recovery will occur only if sensory fibers reach their sensory end targets and motor fibers reach their muscle targets.
The ability to bend the elbow (biceps function) by the one to three months of life is an indicator of probable recovery. Gentle range of motion exercises performed by parents, along with repeated exams by the doctor, may be all that is necessary for patients with strong indicators of recovery.
About two-thirds of children with brachial plexus birth injury get better on their own with minimal treatment. The remaining patients may have limitations related to their brachial plexus birth injury that are not resolving. Limitations may include incomplete range of motion with one or more movements, weak muscles, or decreased sensation (feeling) through the arm. It is for these children that the remainder of our treatment efforts are focused.
The timeframe of surgical repair is an important factor in recovery. Within 18 months, the muscles that have not already connected to nerves may have weakened to the point where it is no longer possible.
For avulsion and rupture injuries, there is no potential for full recovery unless surgical repair is done in a timely manner. For neuroma and neurapraxia injuries, the potential for improvement varies.
If surgery is needed, microsurgical nerve repair may be undertaken as early as three months post injury. Primary nerve repair is typically completed by approximately six months of age following the injury.
Procedures include:
Removal of the constrictive scar tissue surrounding the nerve.
When the neuroma (scar tissue) is large, it must be removed and the nerve is then reattached either with end-to-end techniques or with nerve grafts.
When the gap between the nerve endings is so large that it is not possible to have a tension-free repair using the end-to-end technique, nerve grafting is used.
This is used generally in those cases where there is an avulsion. Donor nerves are used for the repair. The parts of the roots still attached to the spinal cord can be used as donors for avulsed nerves.
Additional procedures are available to improve the overall function of the affected limb.
Procedures include:
Nonsurgical management is also an important part of the treatment process.
Occupational and / or physical therapy is often recommended, including range of motion, strengthening, neuromuscular electrical simulation, kinesio taping, constraint-Induced Movement Therapy (CIMT), serial casting, aquatic therapy and use of orthoses, as needed.
Because your child may not be able to move the affected arm alone, it is important for you to take an active part in keeping the joints limber.
A brachial plexus injury is a lifelong condition. Management often focuses on preventing or minimizing deficits and maximizing the child's capabilities at home and in the community.
It is important to remember that your child is very adaptable. Be supportive and encouraging; focus on what your child can do. Positive reinforcement will help your child to develop a healthy sense of self-esteem and promote independence.
Look up additional information in the brachial plexus glossary.
Our Brachial Plexus Center is one of only a few in the country to offer a team approach to diagnosing and treating children with brachial plexus injuries based on the best scientific information and medical practices available.
Last Updated 02/2024
Learn more about our editorial policy.