
Tracy A. Glauser, MD
- Associate Director, Cincinnati Children's Research Foundation
- Professor, UC Department of Pediatrics
- tracy.glauser@cchmc.org
- Board Certified
About
Biography
I am the associate director of the Cincinnati Children's Research Foundation and a professor of pediatrics at the University of Cincinnati College of Medicine. I received my medical degree, cum laude, from Jefferson Medical College in Philadelphia, PA. I completed my residency in pediatrics at the Johns Hopkins Hospital in Baltimore, MD, and a fellowship in child neurology at The Children’s Hospital of Philadelphia, University of Pennsylvania in Philadelphia, PA. I also completed a National Institute of Neurological Disorders and Stroke research fellowship in pediatric neurology and was a fellow in epilepsy and electroencephalography at St. Louis Children’s Hospital, Washington University School of Medicine in St. Louis, Missouri.
I have authored and co-authored more than 130 articles and book chapters, been involved with the development of six evidence-based guidelines about epilepsy therapy, and given over 150 invited lectures throughout the world. I have been the principal investigator on multiple NIH grants. Currently, I direct the NIH-funded Childhood Absence Epilepsy clinical trial involving 32 pediatric centers around the United States. My fields of expertise are pediatric neurology, pediatric epilepsy, clinical pharmacology, and pharmacogenetics.
MD: Jefferson Medical College, Philadelphia, PA, 1985.
Residency: Johns Hopkins Hospital, Baltimore, MD.
Fellowship: St. Louis Children's Hospital, St. Louis, MO.
Certification: Pediatrics, 1990; Neurology (with special competence in child neurology), 1991.
Interests
Epilepsy; pharmacogenetics; clinical pharmacology
Services and Specialties
Neurology, Epilepsy
Interests
Clinical pharmacology; pharmacogenetics; antiepileptic clinical trials
Research Areas
Neurology, Clinical Pharmacology, Genomics
Location
Insurance Information
Cincinnati Children's strives to accept a wide variety of health plans. Please contact your health insurance carrier to verify coverage for your specific benefit plan.
Publications
Development of information sharing in language neocortex in childhood-onset drug-resistant epilepsy. Epilepsia. 2019; 60:393-405.
Pretreatment behavior and subsequent medication effects in childhood absence epilepsy. Neurology. 2017; 89:1698-1706.
Pretreatment seizure semiology in childhood absence epilepsy. Neurology. 2017; 89:673-679.
Pharmacogenetics of antiepileptic drug efficacy in childhood absence epilepsy. Annals of Neurology. 2017; 81:444-453.
Second monotherapy in childhood absence epilepsy. Neurology. 2017; 88:182-190.
Long-term outcomes of generalized tonic-clonic seizures in a childhood absence epilepsy trial. Neurology. 2015; 85:1108-1114.
Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. The New England Journal of Medicine. 2010; 362:790-799.
A call for solutions-oriented research and policy to protect children from the effects of climate change. Pediatric Research. 2024; 96:1532-1534.
Exome sequencing of 20,979 individuals with epilepsy reveals shared and distinct ultra-rare genetic risk across disorder subtypes. Nature Neuroscience. 2024; 27:1864-1879.
From the Blog
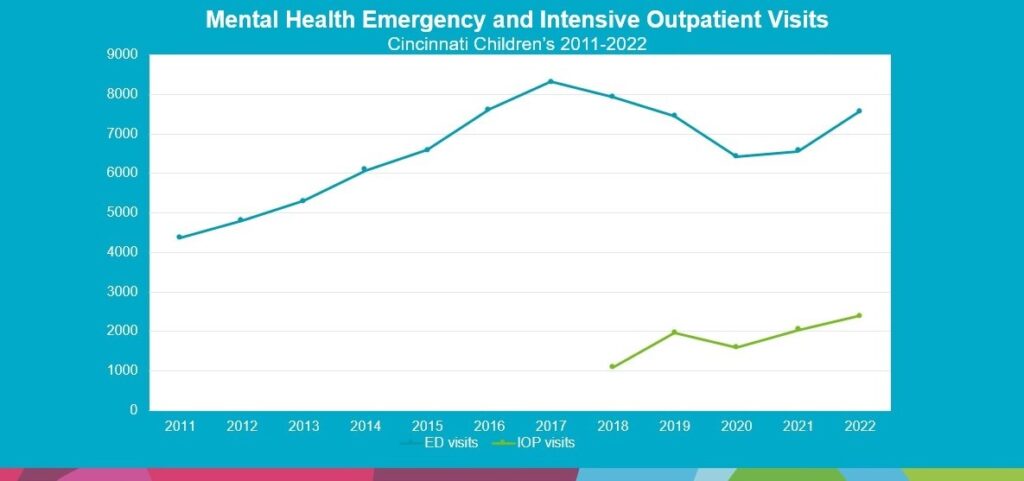
Addressing the Mental Health Crisis Facing Our Youth: Cincinnati Children’s Takes a Proactive Approach
Tracy A. Glauser, MD, Tina L. Cheng, MD, MPH ...5/30/2023
$10M Investment from Cincinnati Children’s Launches Ambitious Mental Health Mission
Tracy A. Glauser, MD, John P. Pestian, PhD, MBA11/8/2021
Digital Providers Surge to Support Global Mental Health During COVID-19 Pandemic
Tracy A. Glauser, MD, John P. Pestian, PhD, MBA2/10/2021
PEDSnet Report Details How COVID-19 Pandemic Has Affected Children
Tracy A. Glauser, MD, Nathan Pajor, MD ...11/23/2020
GRIN Network Shows Early Success in Big-Data Sharing
Tracy A. Glauser, MD9/5/2019










Patient Ratings and Comments
All patient satisfaction ratings and comments are submitted by actual patients and verified by a leading independent patient satisfaction company, NRC Health. Patient identities are withheld to ensure confidentiality and privacy. Only those providers whose satisfaction surveys are administered through Cincinnati Children’s Hospital Medical Center are displayed. Click here to learn more about our survey