- Adherence and Self-Management
- Adolescent Medicine
- Allergy and Immunology
- Anesthesia
- Asthma
- Attention Deficit Hyperactivity Disorder ADHD
- Audiology
- Behavioral Medicine
- Biomedical Informatics
- Biostatistics and Epidemiology
- Bone Marrow Transplantation and Immune Deficiency
- Cancer and Blood Diseases
- Cardiology
- Cardiothoracic Surgery
- Child Abuse Prevention
- Clinical Pharmacology
- Clinical Psychology
- Communication Sciences
- Critical Care
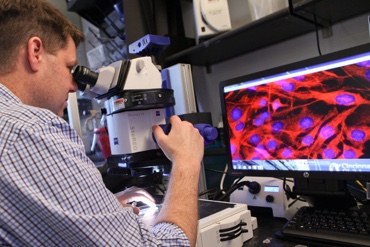
- Developmental Biology
- Developmental and Behavioral Pediatrics
- Emergency Medicine
- Endocrinology
- Eosinophilic Disorders
- Experimental Hematology and Cancer Biology
- Fibrosis
- Gastroenterology Hepatology and Nutrition
- General and Community Pediatrics
- General and Thoracic Surgery
- Genomics
- Global Health
- Gynecology
- Health Technology
- Heart
- Hematology
- Hospital Medicine
- Human Genetics
- Imaging
- Immunobiology
- Infectious Diseases
- Inflammation and Tolerance
- James M Anderson Center for Health Systems Excellence
- Molecular Cardiovascular Biology
- Molecular Immunology
- Neonatology
- Nephrology and Hypertension
- Neurology
- Neuromuscular Development
- Neurosurgery
- Nursing
- Nutrition Therapy
- Occupational Therapy and Physical Therapy Research
- Oncology
- Ophthalmology
- Orthopaedics
- Otolaryngology
- Pathology
- Perinatal Biology
- Pharmacy
- Plastic Surgery
- Prevention of Preterm Birth
- Psychiatry
- Pulmonary Biology
- Pulmonary Medicine
- Quality Improvement
- Radiology
- Rehabilitation
- Reproductive Sciences
- Rheumatology
- Skin
- Sports Medicine
- Urology